Localized Provoked Vulvodynia (LPV) affects up to 28% of women during their lifetime, with around 8% of American women currently experiencing it. LPV is defined as persistent vulvar pain without a clear cause such as infection, skin disease, or other identifiable pathology.

Apply for Free Samples

Apply for Free Samples
What the Research Shows
A 2017 review by Falsetta et al. explored the inflammatory basis of LPV. Researchers found that:
-
Fibroblast cells from the vulvar vestibule in LPV patients were highly responsive to proinflammatory stimuli.
-
These cells produced high levels of pain-related inflammatory mediators, pointing to inflammation as a key contributor to symptoms.
In 2018, the same team expanded on these findings:
-
They discovered that human vulvar fibroblasts express Toll-like receptors (TLRs)—key sensors that trigger immune responses.
-
TLR activation was linked to proinflammatory signaling and chronic pain.
-
Suppressing TLR activity may offer a promising medical treatment pathway.
What This Means for Clinical Care
While pharmacologic approaches targeting inflammation may offer future promise, pelvic physical therapy remains a cornerstone of LPV management.Effective PT interventions include:
-
Desensitization training and graded exposure
-
Manual therapy to release soft tissue restrictions
-
Pelvic floor muscle retraining
-
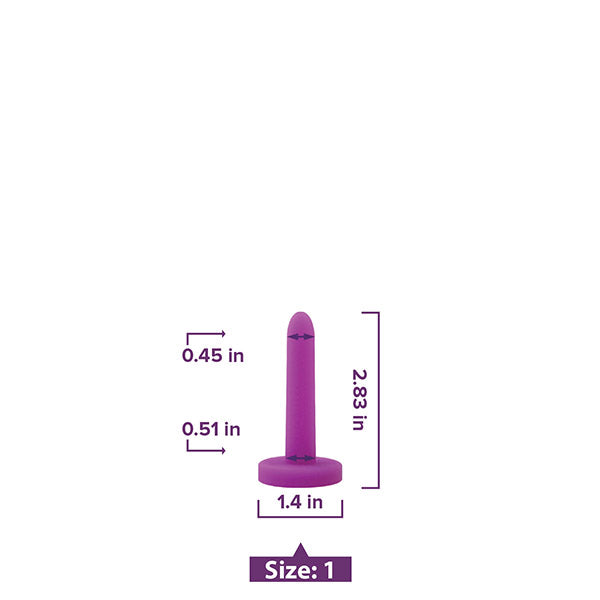
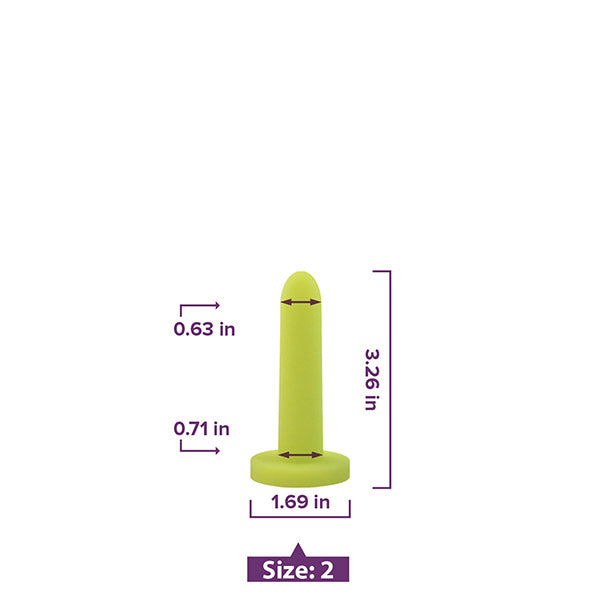
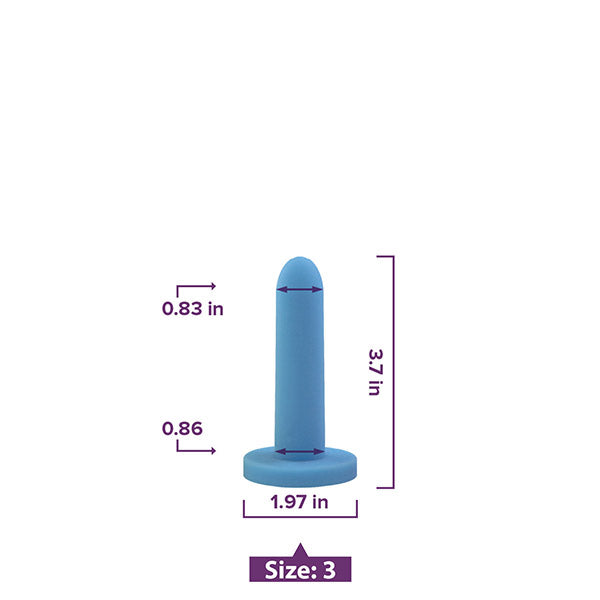
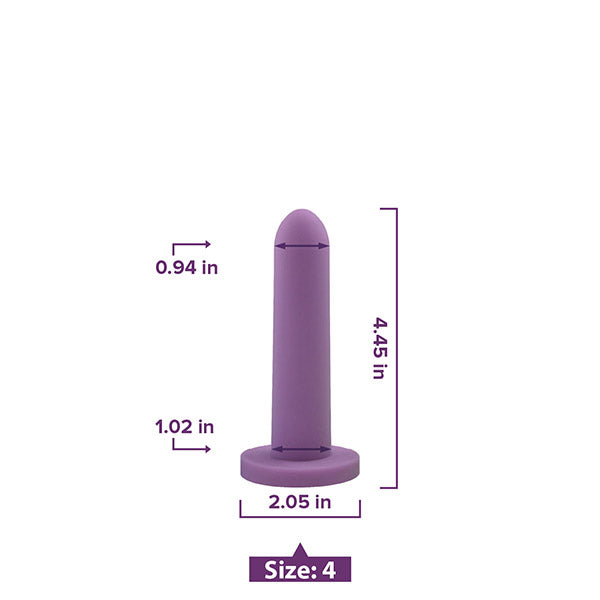
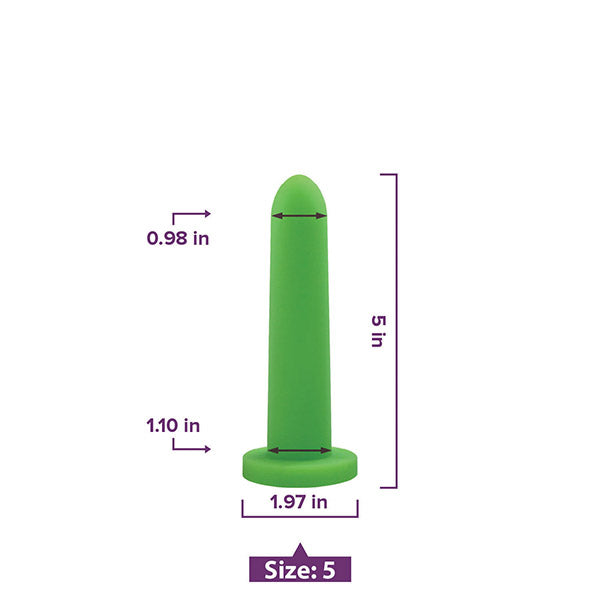
Dilator therapy for vestibular desensitization
-
Lifestyle and pain management education
A Multidisciplinary Approach
LPV is not just a musculoskeletal issue—it’s a complex pain condition with an inflammatory component. Recognizing when to refer patients for medical management of inflammation, while continuing PT care, can lead to better outcomes.- Benkhadra K et al. Menopausal Hormone Therapy and Mortality: A Systematic Review and Meta-Analysis. J Clin Endocrinol Metab. 2015;100(5):1756–1761.
- Salpeter SR et al. Mortality associated with hormone therapy in younger vs older postmenopausal women: A meta-analysis. J Gen Intern Med. 2004;19(8):791–804.
- Boardman HM et al. Hormone therapy for preventing cardiovascular disease in post-menopausal women. Cochrane Database Syst Rev. 2015.
How do Vaginal Dilators Work?


Apply for Free Samples